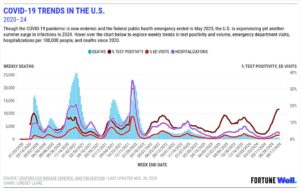
New COVID vaccines are here. What to know about 2024–25 shots as summer surge continues
Citing skyrocketing COVID spread, the FDA announced in late August that it had approved Pfizer’s Comirnaty and Moderna’s Spikevax vaccines early.
As the nation’s biggest summer COVID surge continues—test positivity was projected to be 18% the week ended Aug. 17—help is on the way. The 2024–25 coronavirus vaccines, initially anticipated this fall, are now hitting U.S. clinics, hospitals, pharmacies, and other health care providers.
Back in June, the Centers for Disease Control and Prevention (CDC) recommended everyone ages 6 months and older get an updated vaccine as soon as they became available “later this year.” Last year’s 2023–24 vaccines launched in mid-September, and the public had been expecting the 2024–25 version around the same time this year. Citing skyrocketing disease spread, however, the Food and Drug Administration (FDA) last week announced it had OK’d the vaccines early.
Manufacturers of the two approved COVID vaccines, Pfizer and Moderna, said Aug. 22 that their respective immunizations would be widely available in the days immediately following the FDA’s backing.
In considering vaccination for you and your loved ones, keep in mind the protection you’ll be providing your community, says Dr. Robert Hopkins Jr., medical director of the National Foundation for Infectious Diseases.
“Remember that when you get vaccinated, not only do you give yourself a vaccine that’s going to reduce your risk—short term for infection, longer term for severe infection—that you’re contributing to a community,” Hopkins tells Fortune. “The more people who are vaccinated, the less likely we’re going to get sustained circulation of that virus in the community. That means you’re less likely to get continued evolution of variants.
“It also means fewer people, hopefully, ending up in the hospital or potentially passing away from these viruses. So I think about vaccination for personal benefit, for family benefit, and also for community benefit.”
Who can get a new COVID vaccine?
The CDC recommends a 2024–25 vaccine for everyone 6 months and older—regardless of whether you’ve had COVID, received prior versions of the vaccine, or have never gotten a vaccine. This also includes people who are pregnant or breastfeeding. However, dosage guidelines differ between adults and children:
- Adults 65+
- 1 dose of new Pfizer or Moderna vaccine
- Adolescents and adults 12 to 64
- 1 dose of new Pfizer or Moderna vaccine
- Children 5 to 11
- 1 dose of new Pfizer or Moderna vaccine
- Children 6 months to 4 years
- Never vaccinated
- 3 doses of new Pfizer or 2 doses of new Moderna vaccine
- 1 previous Pfizer dose
- 2 doses of new Pfizer vaccine
- 2+ previous Pfizer doses
- 1 dose of new Pfizer vaccine
- 1+ previous Moderna doses
- 1 dose of new Moderna vaccine
- Never vaccinated
Adults 65 and older, who may be at higher risk of severe COVID infection, were previously advised to get a second dose of the 2023–24 vaccine. For now, the CDC doesn’t recommend a second dose of the 2024–25 vaccine for older adults.
People with moderately to severely compromised immune systems, though, may soon resume eligibility for additional doses. While the CDC hasn’t yet updated its immunization guidelines for this population, they previously were eligible for additional doses at least two months apart. Ask your doctor if you qualify for extra doses.
I recently had COVID. Can I get the new vaccine?
Yes, but you may delay vaccination for up to three months after infection, the CDC says. While you’re less likely to become reinfected so soon after having COVID, research has shown natural immunity to level off after several months.
However, it’s OK to get vaccinated sooner than later if you or a loved one have a medical condition that puts you or them at high risk of severe infection. You may also consider getting vaccinated earlier if the virus is rapidly circulating in your area.
I just got the 2023–24 COVID vaccine. When can I get the new one?
For people 5 and older, the CDC advises postponing your 2024–25 shot until at least eight weeks after your most recent dose of a previous vaccine, including if you were immunized outside the U.S. Children 6 months to 4 years should wait three to eight weeks, depending on their vaccination history; refer to this CDC dosing chart and consult your child’s pediatrician.
If you previously received doses of COVID vaccines that aren’t FDA-approved, FDA-authorized, or prequalified or listed for emergency use by the World Health Organization, the CDC considers you unvaccinated.
Are the Pfizer and Moderna COVID vaccines the same?
Both use messenger RNA (mRNA) technology, and the CDC doesn’t recommend one vaccine over the other. Still, subtleties exist between them.
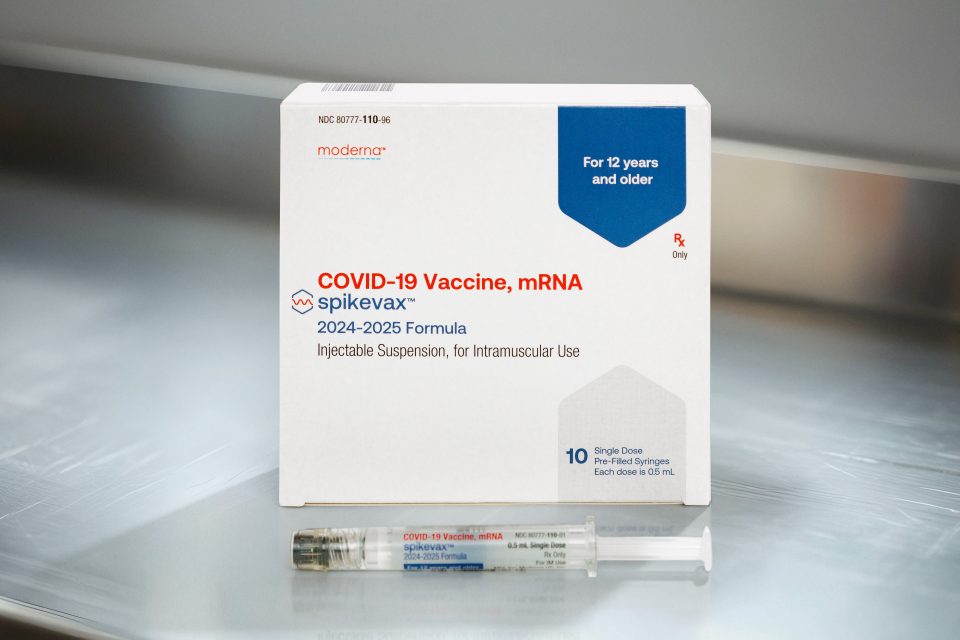
Comirnaty is the brand name of Pfizer’s FDA-approved COVID vaccine for people 12 and older. Each dose contains 30 μg of mRNA. Pfizer’s unnamed version of the vaccine for children 6 months to 11 years has been authorized for emergency use. Single pediatric doses for children 5 to 11 contain 10 μg of mRNA, while doses given in a series for children 6 months to 4 years contain 3 μg of mRNA.
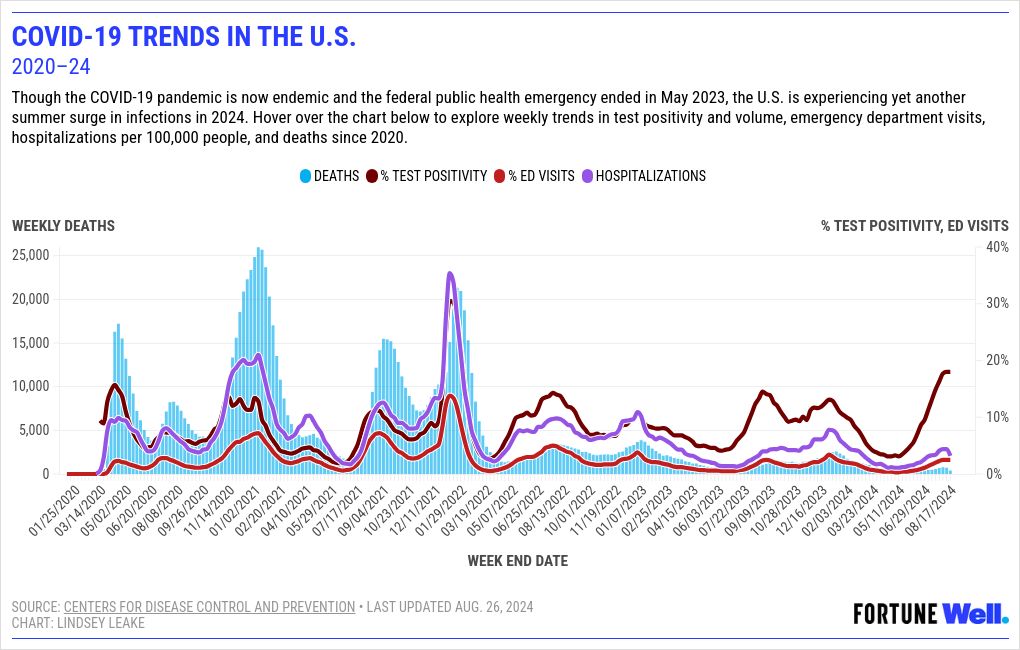
Spikevax is the brand name of Moderna’s FDA-approved COVID vaccine for people 12 and older. Each dose contains 50 μg of mRNA. Moderna’s unnamed version of the vaccine for children 6 months to 11 years has been authorized for emergency use. Single pediatric doses contain 25 μg of mRNA.
All new Pfizer and Moderna vaccines target the Omicron variant KP.2 strain of SARS-CoV-2, the virus that causes COVID.
Courtesy of Moderna
Why isn’t the new Novavax vaccine available yet?
While the Pfizer and Moderna vaccines are mRNA-based, the Novavax vaccine is protein-based. In short, manufacturing the latter is a more complex process, explains Dr. Michael Ben-Aderet, associate medical director of hospital epidemiology at Cedars-Sinai Medical Center in Los Angeles. Despite being newer, the mRNA technology is also relatively swift.
“It uses mRNA, which is a blueprint for a protein, to essentially use your cells to produce the protein that will develop your immunity,” Ben-Aderet tells Fortune. “A protein vaccine is the more traditional way, where you actually give people the protein that you want them to develop immunity to.”
Taking longer to make means protein-based vaccines also take longer to get the FDA’s blessing, he says. Novavax announced last week that the agency was reviewing data in consideration of emergency use authorization for its upcoming vaccine for people 12 and older. The Novavax formula targets JN.1, the parental lineage of KP.2.
I got the shot last year. Do I need the new COVID vaccine?
Yes, the CDC recommends staying up to date with your immunizations. Vaccine-induced immunity decreases over time, so you’re likely not as protected against the coronavirus as you were a year ago. In addition, last year’s vaccine was engineered to combat the most prevalent Omicron subvariants circulating at the time, not the ones now surging and projected to spread through the winter.
In the future, we may even need two or more booster doses per year, says Dr. Priya Sampathkumar, an infectious disease specialist at the Mayo Clinic. But for now, she anticipates the new vaccines will curb the current wave.
“It’s really important that we all get vaccinated prior to cooler weather,” she tells Fortune. “We’ll be moving indoors, [where] there’s a higher risk of transmission.”
Hopkins acknowledges that people may have become apathetic about COVID vaccination more than four years after the virus’s arrival. Yet updated immunization is critical to managing disease spread and severity.
“We had pretty reasonable uptake of the initial round of vaccine. When the bivalent vaccine came out, we saw a dropoff in uptake of that, and a dropoff again in the 2023–24 vaccine,” Hopkins says. “Where that’s left us is that we’ve continued to see thousands of hospitalizations every year due to COVID-19. We’ve continued to see thousands of deaths every year due to COVID-19.
“The absolute numbers have come down from the first year of the pandemic, but it’s still having a major impact on our society.”
Steven Decroos/Pfizer via AP
Can you get COVID from the vaccine?
No. Any post-immunization malaise you may feel is your immune system kicking into gear, Sampathkumar explains.
“It’s technically impossible for the vaccines to [give you COVID],” she says. “What you’re feeling is evidence that the body is responding appropriately…you should welcome that.”
Because younger people have more robust immune systems, they may experience a stronger reaction, she says. In addition, the severity of your reaction should decrease over time. For example, you may not have much of a reaction to your annual flu shot if you’ve been getting it your whole life, but you may have felt poorly after your first COVID shot because it was foreign to your body.
Ben-Aderet adds that COVID vaccines don’t contain virus particles let alone live virus: “All they have in them is a small fragment of mRNA, so there is just no way that that could lead to an infection.”
Can I get the COVID and flu shots at the same time?
Yes, per the CDC. Sampathkumar adds, “It’s absolutely fine getting multiple vaccines at the same visit. It does not decrease your response to any of the vaccines you get.”
Can I still get COVID if I’m vaccinated?
Yes. No vaccine is 100% effective—especially given SARS-CoV-2’s penchant for mutation—and getting immunized doesn’t guarantee you won’t get COVID. Rather, the vaccine’s job is to keep you as healthy as possible if you do become infected, helping prevent severe disease, hospitalization, and death.
Does insurance cover the new COVID vaccine?
The vaccine is free to most U.S. adults through their private health insurance, Medicare, and Medicaid plans, according to the CDC. Children 18 or younger may be eligible for free immunization through the CDC’s Vaccines for Children Program.
The 25 million to 30 million adults nationwide without insurance or whose insurance doesn’t cover all vaccine costs had been offered free COVID immunization through the federal Bridge Access Program, but the initiative was slated to end on an unspecified date this month. CDC Director Dr. Mandy Cohen said in a briefing last week, however, that the agency had earmarked an additional $62 million that would allow state and local immunization programs to purchase vaccines for uninsured and underinsured patients.
“I would encourage folks to be reaching out to their local public health departments, their state public health departments,” Cohen said. “Their federally qualified health centers as well, those are opportunities.”
Where can I get the new COVID vaccine?
Visit Vaccines.gov to find a location near you. You can also call 800-232-0233 or text your ZIP code to 438829.
Do I still need a COVID vaccination card?
If you received your initial COVID vaccine doses when they first became widely available in 2021, you may have a paper, CDC-issued vaccination card. They were once such a hot commodity that retailers offered deals to customers who brandished them and criminals were caught selling fake ones.
The CDC no longer issues these cards, so no need to worry about losing yours or having to bring it to your next vaccination. You may request a paper or digital copy of your vaccine history from your state’s Immunization Information System if you wish.
For more on COVID-19 and vaccines: