An intergenerational epidemic is bubbling beneath America’s maternal mental health crisis
The maternal health crisis is having a knock-on effect on children under 7, writes psychiatrist and LunaJoy co-founder Shama Rathi.
I met “Amelia” early on in my psychiatry practice. It was immediately clear to me that Amelia, at seven years old, was carrying an incredible emotional burden for her young age. Though reluctant at first, Amelia eventually opened up about her home life. She spoke with hesitance about her mother’s “bad days”: the weekends she’d stay in bed, the weeknights she’d spent fighting tears after working long overtime hours, the moments when her seemingly jovial mood would suddenly flip to anger.
With a father who was no longer in the picture, Amelia’s fragile and capricious family life was affecting her behavior both in the classroom and at home. She spoke of trouble making friends, of sleepless nights, and of the weight of responsibility she felt caring for her younger brother after school. She was, above all, hopeful that her mother would “get better.”
Amelia’s mother, I came to learn, was battling postpartum depression (PPD). It’s a broad misconception that PPD vanishes a few months after childbirth. Untreated, the condition can exacerbate into chronic mental illness and depression. This was the case with Amelia’s mother, and it was having a profound impact on the family unit.
Whether we realize it or not, we all know a mother who has experienced a mental health condition during or after pregnancy. One in five individuals struggle with mental health conditions ranging from obsessive-compulsive disorder (OCD) and postpartum psychosis to mood and anxiety disorders and substance use disorders over the course of this period.
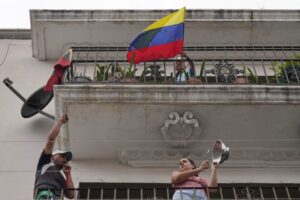
The U.S. is in the midst of a deadly maternal mental health crisis—and it’s causing one in four pregnancy-related deaths every year. Despite its prevalence, this health crisis is poorly understood, under-researched, and continues to magnify as we learn more about it. Just recently, the Biden administration organized a task force to develop recommendations on how to expand equitable access to mental and behavioral health resources for mothers.
The initiative is igniting a broader discourse around maternal mental health. Yet, less discussed is the latent, insidious, and enduring impacts this crisis has had—and continues to have—on American families like Amelia’s.
Maternal mental health and the family unit
As a society, we tend to think about PPD, OCD, and general anxiety disorder as temporary conditions that can crop up during and after pregnancy. Social circles, and even families, are quick to dismiss warning signs as transitory bumps on the road from pregnancy to motherhood—short-term hormonal phenomena that will pass with time. It’s a harmful misconception.
These are serious conditions that can last for years, and the impact they’re having on the development of children is devastating. If one in five mothers are living with mental health conditions associated with maternity, we should presume one in five family units are affected by this crisis, as well.
I see it in my practice on a regular basis; children between the ages of four and seven who are struggling with depression, poor self-esteem, and fractured relationships with their parents.
The behavior of children does not develop in a vacuum. Unfortunately, this is an area of medical research that is tragically understudied. While it is understood that maternal mental health conditions like anxiety and depression are associated with child emotional behavioral problems and can place children at a higher risk of developmental vulnerability, the long-term effects are not as clear.
What we do know is that mothers who have a history of mental health conditions or are genetically predisposed to PPD are much more likely to experience it themselves. We also know that 75% of people with perinatal mental health conditions never receive treatment, leaving them and their families to endure the unknown impacts themselves.
I’ll often ask my patients when they last remember being happy, or if they can recall the last time mom was happy. I’ll ask them to recall the last time they felt connected to their mother. Frequently, the answer is “I can’t remember.” This emotional unavailability disrupts the parent-child connection and can lead to difficulties in emotional regulation for the child. Often, the child acts out as they struggle to manage their feelings, develop unhealthy coping skills, and experience difficulties with cognitive development.
As these children age into adulthood, these challenges evolve into foundational insecurities that skew the way they see the world, themselves, and their relationships.
Our maternal mental health crisis has the makings of a generational epidemic, one that has likely persisted for decades. And while our healthcare system has the tools to stop it in its tracks, it does not yet have the capacity to address it at scale.
Preparing for a solution
Family systems theory suggests family units are single, organized structures made up of interdependent members. Within this structure, a causal factor that impacts one member will reverberate throughout the unit, touching every member. Arguably all of us have experienced the negative factors at least once in our lives, whether it’s a parent losing a job, or a sibling struggling with a health condition. But the theory also applies to positive factors.
In the case of maternal mental health, the idea is that preventative measures for mothers can be impactful for their loved ones.
Most maternal mental health conditions such as general anxiety and PPD can be treated. Where the U.S. has fallen short is in screening for these conditions, as less than 20% of women are ever screened during pregnancy and postpartum.
On the surface, the crisis seems rooted in poor access to diagnostics and preventive care. The Biden administration’s new task force has been charged with developing a strategy to expand access, but the reality is, access is just the first step. What happens to newly diagnosed women when our healthcare system, which is in the midst of a severe shortage of clinical labor, is suddenly overwhelmed with new cases? What happens to mothers when wait times to see a specialist are even worse than they currently are? What happens to their families and children?
New care programs, technologies, and clinical workforce initiatives are necessary. Equally important is a shift in our culture and collective attitudes toward maternal mental health.
Countries in Europe and Asia are increasingly adjusting their understanding of maternity to include the “fourth trimester”—the turbulent 12 weeks following childbirth during which the emotional and physical health of both mother and child undergo incredible changes. This should be a period of rest, rejuvenation, and treatment for American families. If we are able to adopt a forward-looking, well-informed understanding of this period across our social and working lives, our healthcare system’s ability to intervene and deliver necessary care will follow suit.
Healing starts with a holistic understanding of our maternal mental health crisis and its impacts on family units. Millions of mothers are struggling with mental health conditions associated with maternity—and for each one of them, there are children just like Amelia who are hoping their mother gets better.
More must-read commentary published by Fortune:
The opinions expressed in Fortune.com commentary pieces are solely the views of their authors and do not necessarily reflect the opinions and beliefs of Fortune.