Are weight-loss injections the answer to obesity?
The appeal is clear – but should we be turning to appetite-suppressing injections?

You cannot escape the hype around weight-loss injections.
Social media is full of before-and-after pictures. They are the source of wild gossip about Hollywood stars, and now the UK’s National Health Service is going to pay for them.
You can understand the appeal. Excess weight affects our health and leads to stigma – and the mantra of “diet and exercise” has simply failed for most people.
But should we be calling semaglutide, the drug in question, a “miracle” or “skinny jab” when some doctors think it is as controversial as treatments get? Does the hype match the reality? Or are we failing to tackle the causes of obesity and just consigning people to a lifetime of medication?
Jan, from Kent, was one of the first people in the world to take part in the trials of semaglutide. It is sold as Wegovy for weight-loss and as Ozempic for diabetes, although some people have been buying this version to lose weight.
We all know somebody like Jan, who has tried every diet, and she has been battling her waistline her whole life.
Semaglutide mimics a hormone that is released when we eat. It tricks the brain into thinking we are full and dials down appetite so we eat less.
Once Jan started having the injections, her relationship with food was so transformational that she told me it was either down to the drug or “I’ve been abducted by aliens”.
For the first time she could go into a cafe, see some millionaire’s shortbread and not have her body screaming, “I need one”.
Instead it was, “I don’t feel hungry… my body was saying you don’t want it, it wasn’t me using willpower,” she says.
The results of semaglutide are undeniable – at least for a while.
On average, people who were obese lost about 15% of their body weight when taking semaglutide alongside healthy lifestyle advice in a trial. Note this is not a “skinny jab” – 15% takes you from 20 stone down to 17.
That study showed the weight came off over the first year and then stabilised for the remaining three months of the trial. We do not know what happens when people take the drug for years.
Jan lost 28kg (more than four stone). It meant she could finally enjoy her 60th birthday present – a flight in a Tiger Moth aeroplane, having been over the maximum weight limit before. “I was flying in more ways than one, and boy did I enjoy it.”

The results seem more compelling than your typical diet, which often starts well but then your depleted fat stores signal to the brain to seek food. That is why diets ultimately fail.
“More than 90% of people tend to end up back at the weight they were before they started on their dietary journey,” says Prof Sir Stephen O’Rahilly, the director of the Medical Research Council’s Metabolic Diseases Unit.
He sees these drugs as the “beginning of an exciting era” where drugs can help people who have “struggled for a long time” with weight that is damaging their health.
Jan’s trial concluded, and she was no longer able to take semaglutide. Without the drug her brain was no longer being tricked into thinking she was full.
“I was quite upset because the weight was going back on,” she told me – and she was “promising the world” to anybody who could give her the drug.
She tried other weight-loss injections, but ultimately chose to have major surgery and a gastric sleeve to reduce the size of her stomach, so she would feel full faster.
Jan has “no regrets” and still describes the drug as the “best thing that ever happened to me”.
The weight comes back
However, her experience is far from unique and the weight gain after coming off semaglutide is swift. The best long-term data we have shows people regain two-thirds of their lost weight within two years of stopping.
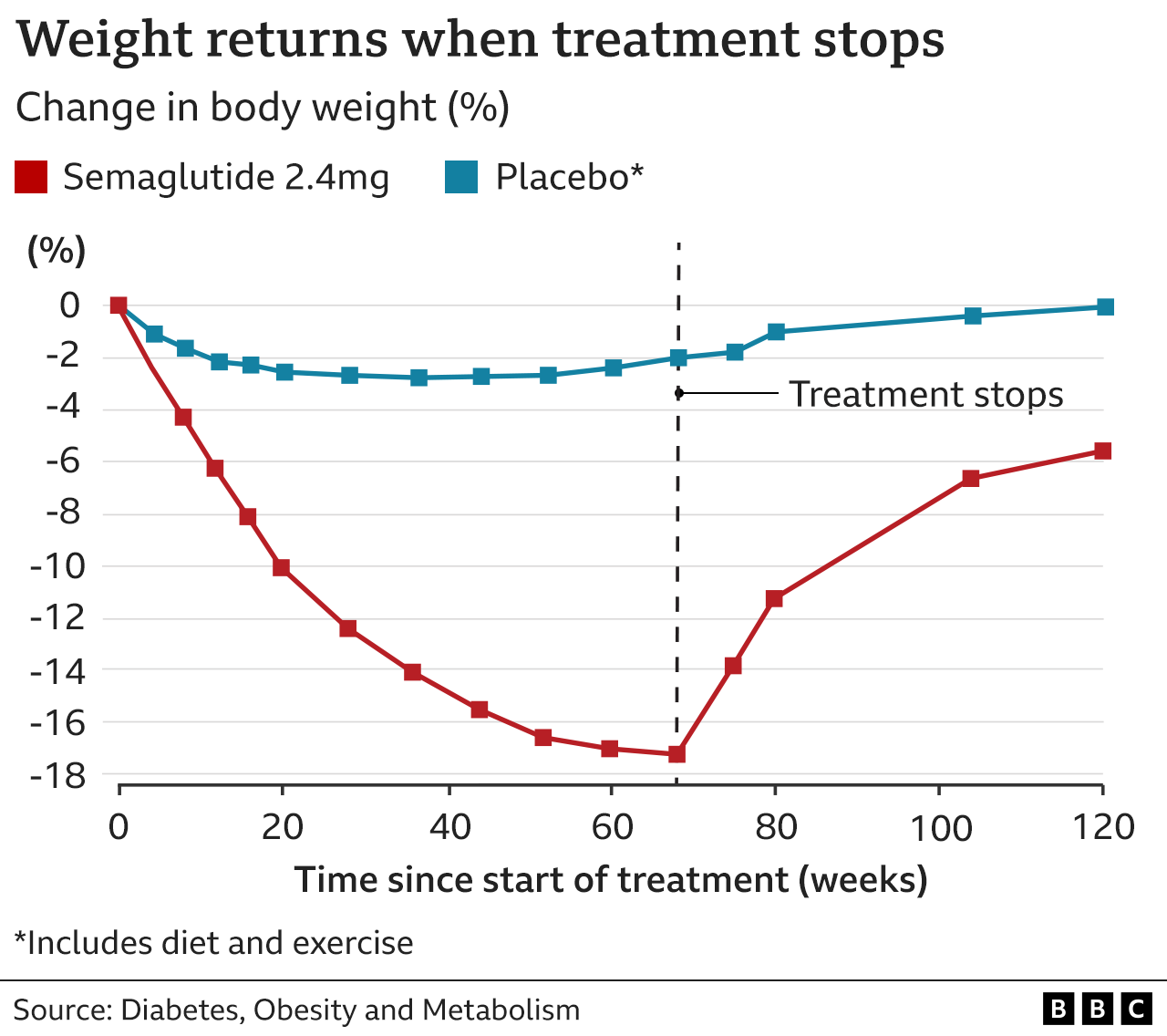
“It’s a drug that seems to need to be kept taken in order to ensure that weight doesn’t return and that’s, for me, a big problem,” says Dr Margaret McCartney, a GP and champion of evidence in medicine.
The NHS is offering semaglutide for only two years, which is how long people can access weight loss clinics. Given the weight gain after coming off the drug, it is fair to ask – what is the point?
“It’s really pretty awful for many people who are wanting to lose weight, and have struggled usually for years. If you get something that ends up working for you, and then for the NHS to go and withdraw that again, it does seem to me to be a bit unfair,” says Dr McCartney.
There are, of course, circumstances where temporarily losing weight may be beneficial. Some surgeries and treatments are only offered to people below a set threshold, for example.
It is a new drug and the long-term safety is unknown. Side effects include vomiting, fatigue and an inflamed pancreas.
Medical victory or societal failure?
Personally, I cannot figure out whether we should celebrate that medicine has produced such a drug, or if it is actually the opposite – that we have failed so badly to tackle obesity throughout society that we now need drugs.
“Many of us have been wrestling with that,” says Naveed Sattar, professor of metabolic medicine at the University of Glasgow.
He comes down on the side of pragmatism. Half the planet is projected to be overweight or obese by 2035, and excess weight is linked to type 2 diabetes, heart disease and some cancers. Cheap calories have “fed into human biology of being tempted by food and overeating”, he says.
And many NHS patients “have four or five conditions as a result of their excess weight, and at the moment we pay lip service to it”, he says.
Meanwhile government obesity policies in the UK – 14 of them in the past three decades – have not turned the tide and that has largely been felt by the poorest people in the country. There is a clear link between deprivation and obesity.
Dr McCartney argues we need to tackle how the world we live in fuels obesity rather than “expecting” people to put on weight “and then accept a medical intervention to treat it”.

-
Listen to Inside Health on BBC Sounds: Is this a new era in tackling obesity?

Semaglutide is changing the landscape of obesity – and alternatives are on the way.
Prof O’Rahilly says that even if we solve the societal causes of obesity “there will be obese people and they will become ill”, so he thinks the drugs will move us to a world of treating obesity “properly as a medical condition”.
But these drugs remain controversial – and we have only discussed their use for improving health.
Further concerns are being raised about the impact on people, often young women, who are pressured to look a certain way when “beautiful” is often equated to “thin”.
The role of celebrity culture, the availability of semaglutide privately through online-only consultations, and the impact on eating disorders are also fuelling questions.
Whatever you think about semaglutide, the debate around this drug, and the hype, is clearly not going away.
Follow James on Twitter. Inside Health was produced by Erika Wright.
More from Inside Health
-
Exercise: What’s the least we can get away with?
-
Multiple sclerosis: Is a virus we all have causing MS?
-
Long Covid: ‘I’ve had long Covid for two years now’

Related topics
-
-
11 February 2021

-